Knee
Knee Anatomy
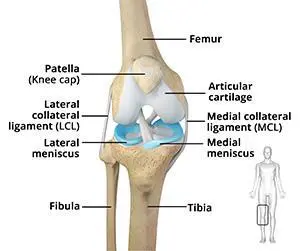
The knee is a complex joint made up of different structures – bones, tendons, ligaments, and muscles. They all work together to maintain the knee’s normal function and provide stability to the knee during movement.
Having a well-functioning healthy knee is essential for our mobility and ability to participate in various activities. Understanding the anatomy of the knee enhances your ability to discuss and choose the right treatment procedure for knee problems with your doctor.

Bones of the Knee
The knee is a hinge joint made up of two bones, the thighbone (femur) and shinbone (tibia). There are two round knobs at the end of the femur called femoral condyles that articulate with the flat surface of the tibia called the tibial plateau. The tibial plateau on the inside of the leg is called the medial tibial plateau and on the outside of the leg, the lateral tibial plateau.
The two femoral condyles form a groove on the front (anterior) side of the knee called the patellofemoral groove. A small bone called the patella sits in this groove and forms the kneecap. It acts as a shield and protects the knee joint from direct trauma.
A fourth bone called the fibula is the other bone of the lower leg. This forms a small joint with the tibia. This joint has very little movement and is not considered a part of the main joint of the knee.
Articular Cartilage and Menisci of the Knee
Movement of the bones causes friction between the articulating surfaces. To reduce this friction, all articulating surfaces involved in the movement are covered with a white, shiny, slippery layer called articular cartilage. The articulating surface of the femoral condyles, tibial plateaus and the back of the patella are covered with this cartilage. The cartilage provides a smooth surface that facilitates easy movement.
To further reduce friction between the articulating surfaces of the bones, the knee joint is lined by a synovial membrane that produces a thick clear fluid called synovial fluid. This fluid lubricates and nourishes the cartilage and bones inside the joint capsule.
Within the knee joint, between the femur and tibia, are two C-shaped cartilaginous structures called menisci. Menisci function to provide stability to the knee by spreading the weight of the upper body across the whole surface of the tibial plateau. The menisci help in load-bearing i.e. it prevents the weight from concentrating onto a small area, which could damage the articular cartilage. The menisci also act as a cushion between the femur and tibia by absorbing the shock produced by activities such as walking, running and jumping.
Ligaments of the Knee
Ligaments are tough bands of tissue that connect one bone to another bone. The ligaments of the knee stabilize the knee joint. There are two important groups of ligaments that hold the bones of the knee joint together, collateral and cruciate ligaments.
Collateral ligaments are present on either side of the knee. They prevent the knee from moving too far during side to side motion. The collateral ligament on the inside is called the medial collateral ligament (MCL) and the collateral ligament on the outside is called the lateral collateral ligament (LCL).
Cruciate ligaments, present inside the knee joint, control the back-and-forth motion of the knee. The cruciate ligament in the front of the knee is called anterior cruciate ligament (ACL) and the cruciate ligament in the back of the knee is called posterior cruciate ligament (PCL).
Muscles of the Knee
There are two major muscles in the knee – the quadriceps and the hamstrings, which enable movement of the knee joint. The quadriceps muscles are located in front of the thigh. When the quadriceps muscles contract, the knee straightens. The hamstrings are located at the back of the thigh. When the hamstring muscles contract, the knee bends.
Tendons of the Knee
A tendon is a tissue that attaches a muscle to a bone. The quadriceps muscles of the knee meet just above the patella and attach to it through a tendon called the quadriceps tendon. The patella further attaches to the tibia through a tendon called the patella tendon. The quadriceps muscle, quadriceps tendon, and patellar tendon all work together to straighten the knee. Similarly, the hamstring muscles at the back of the leg are attached to the knee joint with the hamstring tendon.
ORTHOBIOLOGICS FOR KNEE PAIN
The Healthy Knee
The knee is made up of four bones. The femur or thighbone is the bone connecting the hip to the knee. The tibia or shinbone connects the knee to the ankle. The patella (kneecap) is the small bone in front of the knee and rides on the knee joint as the knee bends. The fibula is a shorter and thinner bone running parallel to the tibia on its outside. The joint acts like a hinge but with some rotation.
The knee is a synovial joint, which means it is lined by synovium. The synovium produces fluid lubricating and nourishing the inside of the joint. Articular cartilage is the smooth surfaces at the end of the femur and tibia. It is the damage to this surface which causes arthritis.
Knee Injuries
Any injury or disease of the knee will adversely affect the joint’s range of motion. The most common knee injuries/diseases include
- Knee Arthritis
- Ligament Tear
- Meniscal Tear
- Patellar Tendinitis
- Patellofemoral Instability
- Cartilage Injury
Progenitor Cells
Progenitor cells are present in all of us acting like a repair system for the body. However, with increased age sometimes the optimum amounts of these cells are not delivered to the injured area. The goal of orthobiologic treatment is to amplify the natural repair system of the patient’s body.
Preparing for the Procedure
It is important that you stop taking any non-steroidal anti-inflammatory drugs (NSAIDs) at least two weeks before your procedure.
Preparing for a orthobiologic procedure is relatively easy and your doctor will give you specific instructions depending on your condition.
Orthobiologic Procedure
The procedure begins with your doctor extracting progenitor cells, and growth factors from either your blood (PRP/PRF), bone marrow, or adipose tissue (fat). After the tissue is harvested it is cleaned and then separated using sterile processing. It is then ready to be used to heal your injured joint or soft tissues.
Your doctor then cleans and numbs your affected area to be treated and then, under the guidance of special x-rays, injects the concentrate into the diseased region. The whole procedure usually takes less than one hour and you may return home on the same day of the procedure.
Post-Operative Care
- You will most likely be able to return to work the next day following your procedure.
- You will need to take it easy and avoid any load bearing activities for at least two weeks following your procedure.
- You will need to refrain from taking non-steroidal, anti-inflammatory medications (NSAIDS) for a while as this can affect the healing process of your body.
Risks and Complications
This Procedure is generally considered a safe procedure with minimal complications, however, as with any medical procedure, complications can occur.
Some of the complications related to ortho biologic therapy include pain at the donor site which usually resolves in 2 to 3 days, swelling at the injection site, bruising at the donor site, bleeding and stiffness. There is a very small risk of infection following these injections which in my experience is much less than 1%.